Translate this page into:
Epidemiology of adolescents and young adult cancers in National Institute of Cancer Research and Hospital, Dhaka

*Corresponding author: Abdullah Al Mamun Khan, Department of Medical Oncology, Shaheed Suhrawardy Medical College Hospital, Dhaka, Bangladesh. mamun3737@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khan AA, Akhtar PS, Ali MY, Khatun N, Alam MJ. Epidemiology of adolescents and young adult cancers in National Institute of Cancer Research and Hospital, Dhaka. Int J Mol Immuno Oncol 2021;6(1):11-5.
Abstract
Objectives:
Cancers in adolescents and young adult (AYA) are increasing day by day but there are few clinical and epidemiological data from developing country. The objectives of the study were to find out disease patterns of cancers in AYA, their relation with age group, sex ratio, and histology.
Material and Methods:
The study was an observational study. All histologically confirmed cancer patients aged 15–39 years registered in NICRH from January 2016 to December 2016 (12 months) were included. The patients were grouped according to Birch classification of AYA cancer. Each patient was interviewed and clinical information and demographic profiles were recorded. Clinical information was retrospectively studied.
Results:
A total of 400 patients were enrolled for this study. Of them, male (M) was 277 (69.25%), female (F) was 123 (30.75%) and male female ratio was 2.25:1. Younger AYA patients (15–19 years) were most common, 126 (31.50%). Then, next common was young adult (35–39 years), 102 (25.50%). Remaining age group patients 20–24 years, 25–29 years, and 30–34 years group were 50 (12.50%), 57 (14.25%), and 65 (16.25%), respectively. The six most common cancers were germ cell tumor (GCT) and trophoblastic tumor 64 (16%), lymphomas 63 (15.75%), osseous and chondromatous neoplasm 63 (15.75%), soft-tissue sarcoma (STS) 55 (13.75%), leukemia 50 (12.50%), and gastrointestinal tract (GIT) carcinoma 46 (11.5%). The most common cancers in younger AYA (15– 19 years) were osseous and chondromatous neoplasm 38 (30.16%), leukemia 27 (21.43%), STS 26 (20.63%), and in contrast, older AYA (35–39 years) suffered mainly from lymphoma 21 (20.59%), GIT carcinomas 20 (19.61%), and GCT and trophoblastic tumor 19 (18.63%). The leading cancers in 20–24 years aged group were bone tumor 12 (24%), GCT and trophoblastic tumor 12 (24%), and STS 9 (18%); 25–29 years aged group were lymphoma 10 (17.54%), STS 9 (15.79%), and GIT malignancy 9 (15.79%); 30–34 years aged group were GCT and trophoblastic 21 (32.31%), lymphoma 15 (23%), and GIT cancer 8 (12.31%). The leading presenting features were swelling 177 (44.25%), pain 122 (30.50%), fever 110 (27.5%), vomiting 65 (16.25%), loss of appetite 60 (15%), and bleeding manifestations 30 (7.5%). Majority 146 (36.50%) were educated up to primary, 50.50% of patients belongs to low socioeconomic status, 25.25% was student, 64.50% was rural dweller, and 39.50% and 33.00% presented with Stage iv and Stage iii, respectively, among them 47.75% with performance status Grade 2 according to Eastern Cooperative Oncology Group.
Conclusion:
In AYA, the six most common cancers were GCT and trophoblastic tumor.
Keywords
Adolescents and young adults
Cancer
Epidemiology
Bangladesh
INTRODUCTION
The discipline of adolescent and young adult oncology (AYAO) is an evolving field that has begun to be defined only within the last decade. The increasing focus over the past 10 years on the outcomes, unique challenges of care, and distinct biology of young adult cancers is beginning to stimulate interest in the development of clinical programs specific to the care of AYA cancers. Cancer is regarded as a disease of older adults with cancer of colon, breast, lungs, and prostate constitutes the major cancers. Little is known and reported in literature about the incidence and patterns of this disease in AYA. This population poised between children and adults has been called the “lost tribe.”[1]
While the incidence of cancer in AYA is lesser than that in older adults, the population pyramid of developing countries is predominantly young [Figure 1].[2]

- Population pyramid Bangladesh.
There are very few studies in developing countries and also in Bangladesh, with AYA malignancies. There are also limited studies and literatures available in developing countries. The annual number of AYA cancers, although small, will constitute a significant burden. This diagnosis disrupts the normal trajectories of development including physical, psychological, social, and life goals related to family and careers. For this reasons, cancer in AYA merits attention. The study for AYA first started 1978 in the UK. After a long gap, the studies are running from 2005 in few countries, especially in Canada, the USA, and India.[3] Causes of AYAs are unknown. The risk factors of AYAs are not understand clearly also. They present with multiple clinical features such as swelling, pain, fever, nausea, and vomiting. Early detection of the disease by recognizing signs and symptoms that appeared first will be beneficial for the patients with AYA tumor as prognosis differs with the stage of the disease. Although cancer is the second leading cause of death in AYA (12% of death), it is still relatively uncommon. The incidence of cancer is increasing. Fortunately, with modern aggressive multidisciplinary therapy, 5-year survival for this group with cancer exceed 75% in the USA.[4]
This age range is characterized by marked hormonal and physiologic changes, as well as significant psychological and sociocultural transitions such as attending college, starting a career or family, or caring for aging parents. These transitions bring additional considerations into cancer treatment decisions, such as lack of insurance, fertility preservation, and logistical challenges that can contribute to delays in diagnosis and lack of adherence to care plans that are often not issues for older or younger patient populations. The age limit of this study was 15–39 years. Our objective was to study the descriptive epidemiology of cancers in AYAs at NICRH and to compare this with the available data in other countries literature. About 70,000 young people (ages 15–39) are diagnosed with cancer each year in the United States – accounting for about 5% of cancer diagnoses in the United States. This is about 6 times the number of cancers diagnosed in children ages 0–14 years.[5] There is no study in Bangladesh with AYAs malignancies in older AYAs. There are limited studies and literatures are available from developed countries. The annual number of AYA cancers, although small, will constitute a significant burden. There are 72,006,601.45 (44.2%) people under this 15–39 years age group.[6] They are in vital age group not only for their own development but also for their country.
MATERIAL AND METHODS
This study was designed as an observational study from January 2016 to December 2016 for a period of 12 months. All the diagnosed case of cancers, at the age of 15–39 years, take treatment or admitted in the Department of Medical Oncology, Pediatric oncology, Hemato-oncology and Radiation oncology of NICRH were selected as study population. The sample was collected by purposive sampling technique using inclusion and exclusion criteria. All data were recorded systematically. Age- and gender-specific distribution of tumors in AYA was showed as per Birch classification.
RESULTS
Demographic profile of AYA cancer patients showed maximum 126 (31.50%) patient distributed in 15–19 years age group followed by 102 (25.50%), 65 (16.25%), 57 (14.25%), and 50 (12.50%) in 35–39 years, 30–34 years, 25–29 years, and 20–24 years, respectively. On both side of these age groups, the number of the patient was raised. Male (277) was predominant than female (123) (Male:female = 2.25:1). Maximum patients were educated up to primary level 146 (36.50%). Comorbidities were seen only in 26 AYA patients like diabetes mellitus (DM) 9 (2.25%), chronic obstructive pulmonary disease (COPD) 7 (1.75%), hypertension 4 (1%), hemorrhoid 3 (0.75%), bronchial asthma 2 (0.5%) and epilepsy 1 (0.25%) [Figure 2 and Table 1].
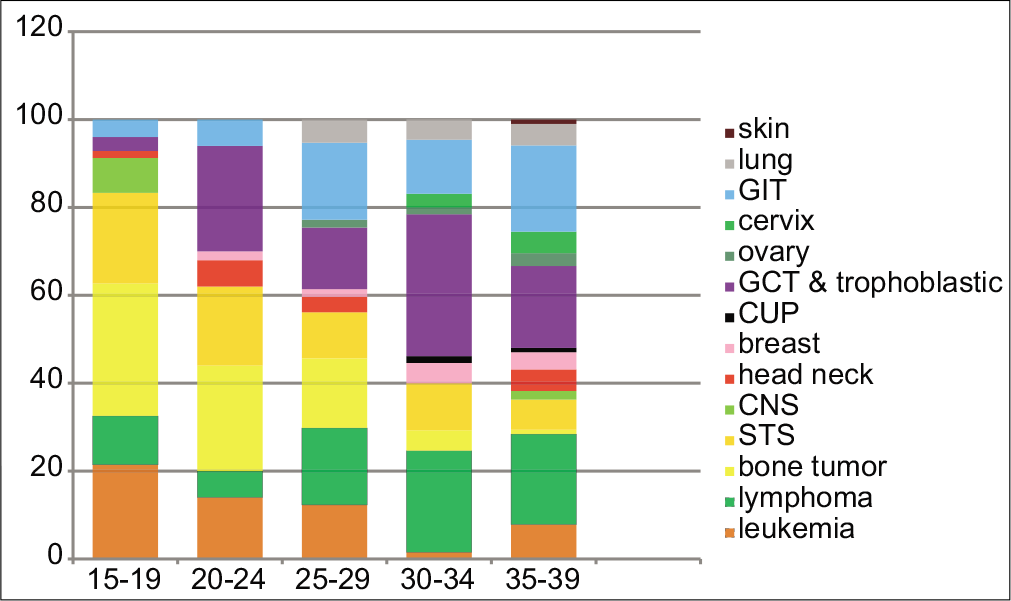
- Types of adolescents and young adult cancers (% cases) and age at diagnosis.
| Birch classification | Male total | Female total | Age group 15–19 | Age group 20–24 | Age group 25–29 | Age group 30–34 | Age group 35–39 | Total |
|---|---|---|---|---|---|---|---|---|
| Group 1 – leukemia | ||||||||
| 1.1 ALL | 12 | 8 | 14 | 5 | 1 | 00 | 00 | 20 |
| 1.2. AML | 16 | 6 | 13 | 1 | 3 | 1 | 4 | 22 |
| 1.3. CML | 6 | 2 | 00 | 1 | 3 | 00 | 4 | 8 |
| Group 2 – lymphoma | ||||||||
| 2.1 HL | 20 | 10 | 7 | 1 | 3 | 9 | 10 | 30 |
| 2.2 NHL | 24 | 9 | 7 | 2 | 7 | 6 | 11 | 33 |
| Group 3 – CNS tumor | ||||||||
| 3.1 Astrocytoma | 2 | 1 | 3 | 00 | 00 | 00 | 00 | 3 |
| 3.2 Medulloblastoma | 2 | 00 | 00 | 00 | 00 | 00 | 00 | 2 |
| 3.3 Other unspecified | 5 | 2 | 4 | 00 | 00 | 00 | 3 | 7 |
| Group 4 – Bone tumor | ||||||||
| 4.1 Osteosarcoma | 31 | 8 | 18 | 12 | 5 | 3 | 1 | 39 |
| 4.2 Chondrosarcoma | 2 | 1 | 00 | 3 | 00 | 00 | 00 | 3 |
| 4.3 Ewing sarcoma | 16 | 5 | 15 | 4 | 2 | 00 | 00 | 21 |
| Group 5 – STS | ||||||||
| 5.1 RCT | 4 | 2 | 5 | 1 | 00 | 00 | 00 | 6 |
| 5.2 Fibrous histocytoma | 5 | 1 | 00 | 1 | 1 | 2 | 2 | 6 |
| 5.3 Fibrosarcoma | 6 | 00 | 2 | 1 | 2 | 1 | 00 | 6 |
| 5.4 Synovial sarcoma | 4 | 1 | 5 | 00 | 00 | 00 | 00 | 5 |
| 5.5 MPNST | 5 | 00 | 2 | 1 | 00 | 1 | 1 | 5 |
| 5.6 PNET | 2 | 1 | 3 | 00 | 00 | 00 | 00 | 3 |
| 5.7 Myxosarcoma | 1 | 1 | 1 | 1 | 00 | 00 | 00 | 2 |
| 5.8 Liposarcoma | 1 | 1 | 00 | 1 | 1 | 00 | 00 | 2 |
| 5.9 Other STS | 15 | 5 | 12 | 5 | 2 | 00 | 1 | 20 |
| Group 6 – GCT and trophoblastic | ||||||||
| 6.1 Gonadal | 48 | 1 | 1 | 12 | 8 | 20 | 10 | 51 |
| 6.2 Non-gonadal | 3 | 12 | 3 | 00 | 00 | 1 | 9 | 13 |
| Group7 – Melanoma/skin | ||||||||
| 7.1 Skin cancer | 1 | 00 | 00 | 00 | 00 | 00 | 1 | 1 |
| Group 8 – Carcinoma (except skin) | ||||||||
| 8.1 Carcinoma head-neck | 11 | 1 | 2 | 3 | 2 | 00 | 5 | 12 |
| 8.2 Carcinoma lung | 10 | 1 | 00 | 00 | 3 | 3 | 5 | 11 |
| 8.3 Carcinoma breast | 00 | 9 | 00 | 1 | 1 | 3 | 4 | 9 |
| 8.4 Carcinoma GIT | 00 | 9 | 00 | 1 | 1 | 3 | 4 | 9 |
| 8.5 Gynecological malignancy | 36 | 10 | 5 | 3 | 10 | 8 | 20 | 46 |
| Ovary cancer | 00 | 5 | 00 | 00 | 1 | 1 | 3 | 5 |
| Cervical cancer | 00 | 7 | 00 | 00 | 00 | 2 | 5 | 7 |
| Group 9 – unspecified malignant neoplasm (CUP) | 2 | 00 | 00 | 00 | 00 | 1 | 1 | 2 |
| Total | 277 | 123 | 126 | 50 | 57 | 65 | 102 | 400 |
The leading clinical feature was swelling 177 (44.25%), followed by pain 122 (30.50%), fever 110 (27.50%), loss of appetite 60 (15%), bleeding manifestations 30 (7.5%), and weight loss 10 (2.25%). Risk factors including tobacco 69 (81.17%) for lung, head-neck, cervical, and GIT cancer, 5 (71.43%) patients were married at early age* that were risk for cervical cancer, chemical or dust exposure 5 (41.66%) for lung and skin cancer, welding machine exposure 3 (27.27%) for lung cancer, and undescended testes 1 (1.96%) for testicular carcinoma. Smoking was present among 79 (19.75%). There were 29 (7.25%) patients who were used to betel nut and jarda followed by gul 6 (1.0%) and addicting drugs 3 (0.75%).
Majority 126 (31.50%) of patients were young AYA (15–19 years), then old AYA (35–39 years) group, 102 (25.50%). Remaining age group patients, 20–24 years, 25–29 years, and 30–34 years group were 50 (12.50%), 57 (14.25%), and 65 (16.25%), respectively. Regarding the Birch classification of cancers in AYA, germ cell tumor (GCT) and trophoblastic tumor 64 (16.00%) griped in the majority of the respondents in Group 6 followed by lymphoma 63 (15.75%) in Group 2 and bone tumor 63 (15.75%) in Group 4. It was revealed that regarding Group 1, majority were 22, among them, majority were in the age group of 15–19 years followed by ALL (20). Regarding Group 2, highest number (33) was NHL, among them, majority (11) belonged in the 35–39 years age group followed by HL (30) in which majority was also in same age group. Regarding Group 8, highest (46) was gastrointestinal tract (GIT) malignancy, among them, majority (24) were in the age group of 35–39 years, head-neck cancer 12 (3%), breast cancer was 9 (2.25%), cervical cancer 7 (1.75%), and ovary cancer were 5 (1.25%). Regarding Group 7, only one patient had been suffering from skin cancer.
According to performance status, 191 (47.75%) patients of AYA were with Eastern Cooperative Oncology Group (ECOG) Grade 2 performance status, 109 patients (27.25%) were in ECOG Grade 1 and only (12.3%) were in Grade 0. Maximum number of patients, that is, 158 (39.5%) came with Stage IV disease, whereas 50 patients (12.5%) came with Stage I disease and 132 (33%) patients came with Stage III and 60 (15%) patients with Stage II disease. Two hundred and fifty-eight (64.5%) patients came from rural area and 136 (34%) patients were dweller of urban area. Regarding occupation of AYA patients, students were 101 (25.25%), house wife 97 (24.25%), service 72 (18%), business 51 (12.75%), farmer 40 (10%), occupation less 14 (3.5%), welding and electrician 9 (2.25%), and Only 1 (0.25%) was street beggar.
DISCUSSION
This study was compared with the studies abroad like India,[9,10] international reported series,[5] the UK data set,[11] Korean hospital-based cancer registry (HBCR),[12] and the Netherlands HBCR.[8] By comparing this study with others studies, it was documented that the disease pattern of AYA in different geographical variation was different according to disease prevalence. Ten most common malignancies in Bangladesh among the said age group were (1) GCT and trophoblastic tumor, (2) lymphoma, (3) osseous and chondromatous sarcoma, (4) soft-tissue sarcoma, (5) leukemia, (6) GIT malignancy, (7) GTT, (8) head-neck malignancy, (9) breast cancer, and (10) lung cancer [Table 2].
| Netherlands National PBCR, n=23,161, 1989–2009[7] | Korea National HBCR, n=39,369, 1999–2010[8] | Max cancer center, India n=287, January-December 2014 | SEER Cancer Statistics Review 1975–2011 | Our study result |
|---|---|---|---|---|
| Melanoma | Carcinoma thyroid | Carcinoma GIT | Leukemia | GCT and trophoblastic |
| Gonadal germ cell and trophoblastic | Carcinoma GIT | HL | GIT | Lymphoma |
| HL | Carcinoma genitourinary tract | Carcinoma genitourinary tract | Melanoma and skin cancer | Osseous and chondromatous sarcoma |
| NHL | NHL | GCT and trophoblastic | GCT and trophoblastic | STS |
| Carcinoma genitourinary tract | Carcinoma breast | Carcinoma thyroid, carcinoma head-neck | CNS tumor | Leukemia |
CONCLUSION
The patterns of malignancies and demographic distribution in the AYA cancer patients vary among different countries across the world. This research work revealed that early aged leading malignancies were non-epithelial and late aged AYA cancers were epithelial. GCT, TT, lymphoma, leukemia, and sarcoma were leading malignancies in Bangladesh, whereas GIT, HL, GU malignancy, GCT and TT, and head-neck cancer were leading in India; thyroid, GIT, GU, NHL, and breast cancer were leading in Korea; melanoma, GCT and TT, HL, NHL, and GU malignancies were leading in the Netherlands. It believes that a major specific research initiative emphasizing AYA clinical trials and outcomes research is urgently needed. Collaboration and support from numerous governmental, academic, public health, community based, and other private sector entities will be essential to its success.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Adolescent oncology-a homeland for the lost tribe. Eur J Cancer. 2003;39:2571-2.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of cancers among adolescents and young adults from a tertiary cancer center in Delhi. Indian J Med Paediatr Oncol. 2016;37:90-4.
- [CrossRef] [Google Scholar]
- Population Enumeration Data; Five-Year Age Group Data C-14 Tables. 2014. Available from: http://www.censusindia.gov.in/2011census/c-series/c-14.html [Last accessed on 2014 Nov 20]
- [Google Scholar]
- 2014. Available from: http://www.who.int/topics/adolescent_health/en [Last accessed on 2014 Nov 20]
- Cancer Epidemiology in Older Adolescents and Young Adults 15-29 Years of Age, Including SEER Incidence and Survival: 19752000 Bethesda, MD: National Cancer Institute; 2006.
- [Google Scholar]
- 2016. Available from: http://www.populationpyramid.net
- Cancer in adolescents and young adults (15-29 years): A population-based study in the Netherlands 1989-2009. Acta Oncol. 2012;51:922-33.
- [CrossRef] [PubMed] [Google Scholar]
- Classification and incidence of cancers in adolescents and young adults in England 1979-1997. Br J Cancer. 2002;87:1267-74.
- [CrossRef] [PubMed] [Google Scholar]
- Patterns of Malignancies in Adolescents and Young Adults in Tertiary Care Center from Developing Country, Implication for Outcome Optimization and Health Service SIOP.
- [Google Scholar]
- Pattern of cancer in adolescent and young adults-a ten year study in India. Asian Pac J Cancer Prev. 2010;11:655-9.
- [Google Scholar]
- Cancer at ages 15-29 years: The contrasting incidence in India and England. Pediatr Blood Cancer. 2012;58:55-60.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer incidence and survival among adolescents and young adults in Korea. PLoS One. 2014;9:e96088.
- [CrossRef] [PubMed] [Google Scholar]






