Translate this page into:
Patient perspectives on living with chronic myeloid leukemia in India: Quality of life, psychosocial support, and stigma

*Corresponding author: Satya Sadhan Sarangi, Department of Medical Oncology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India. satyasarangi1991@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sarangi SS, Yadav R, Singh R. Patient perspectives on living with chronic myeloid leukemia in India: Quality of life, psychosocial support, and stigma. Int J Mol Immuno Oncol. doi: 10.25259/IJMIO_17_2024
Abstract
Chronic myeloid leukemia (CML) stands a frequently encountered type of blood cancer. Despite advancements in treatment, CML patients in India encounter obstacles in accessing healthcare and managing treatment-related side effects. This review focuses on understanding the experiences of patients living with CML in India. It delves into various aspects, such as their quality of life, the psychosocial support they receive, and the stigma they might face due to their condition. Psychological, emotional, and financial burdens are significant, compounded by limited social support and stigma. Coping strategies and psychosocial interventions play crucial roles in addressing these challenges. In addition, the review underscores the importance of patient-centred care and advocacy in enhancing outcomes and addressing unmet needs in CML management. Understanding the experiences of patients living with CML informs strategies for improving healthcare services and support systems to ensure holistic care and a better quality of life for patients.
Keywords
Chronic myeloid leukemia
Tyrosine kinase inhibitors
Quality of life
Psychosocial support
Stigma
INTRODUCTION
Chronic myeloid leukemia (CML) is a commonly encountered blood cancer caused by genetic mutations that affect the hematopoietic stem cells in the bone marrow.[1,2] The prevalence of CML in India is approximated to be 5.47/100,000 individuals annually.[3] Consequently, there has been a substantial rise in the incidence of CML, with projections suggesting a potential stabilization by the year 2050.[4] CML was previously considered fatal, but now, there is renewed hope for longer life expectancy and advanced techniques to evaluate this extended longevity.[5] This shift will have a significant effect on the patient’s quality of life, as well as their emotional and cognitive perception of the illness.[5] The life expectancy of patients with CML has substantially improved since the introduction of tyrosine kinase inhibitors (TKIs) in recent decades.[6] TKIs represent the established treatment protocol for recently diagnosed chronic CML patients across all stages of the disease.[7]
Frequently encountered side effects from TKI treatment were diverse, encompassing both physical and psychological manifestations. Physical symptoms often comprised nausea, vomiting, pain, skin issues, and fatigue. Both medication and the disease itself were noted to disrupt daily routines, usual activities, and treatment adherence. Psychological impacts included feelings of low mood, increased attentiveness to general health, and changes in self-perception, marked by reduced confidence and the shift from being seen as an individual to being identified primarily as a patient.[8] Although patients diagnosed with CML have access to effective treatments to manage their condition, many still struggle to maintain a typical quality of life due to the negative impact of prolonged treatment on their overall well-being.[9]
In light of these considerations, this review focuses on understanding the experiences of individuals living with CML in India. It delves into various aspects such as their quality of life, the support they receive, both emotionally and socially, and the stigma they might face due to their condition. Living with CML can significantly affect patients’ emotions and overall well-being. The constant management of symptoms, side effects of treatment, and uncertainty about the disease’s progression can lead to anxiety, depression, and decreased quality of life.
By examining these perspectives, this review helps to gain insight into the challenges faced by CML patients in India and identify areas for improvement in healthcare services and support systems.
UNDERSTANDING CML
Challenges faced by patients in accessing healthcare and treatment in India
While there have been advancements in treating CML that have benefited patients globally, not all regions have experienced these improvements equally. Specifically, countries within the South Asian Association for Regional Cooperation face unique challenges that impede the effective treatment of this hematological malignancy. Limited access to specialized healthcare services and essential medications stands as a primary obstacle for CML patients in this region.[10]
In oncology centers across India, newly diagnosed CML patients are typically started on imatinib.[1] Despite advancements in the survival rates of CML patients, specific obstacles within the Indian healthcare system persist. Patients in India often present with more advanced stages of the disease, exacerbating the challenges of treatment. While imatinib is commonly accessible as the primary treatment in many medical centers, there is a notable scarcity of resources for molecular monitoring and second-line therapy options.[11] This scarcity not only hampers effective disease management but also complicates long-term care provision. Patients’ extended lifespans pose new challenges, such as ensuring continuous drug availability and strict adherence to medication regimens. In addition, managing long-term physical and psychological issues becomes paramount, especially in pediatric cases where the impact can be particularly profound. Some patients may not tolerate imatinib or face treatment failure, necessitating the use of more expensive second-line TKIs.[1] Addressing these challenges requires a comprehensive approach that considers both immediate treatment needs and long-term care requirements.
Impact of CML on patients’ daily lives, relationships, and livelihoods
CML affects the daily lives of patients in profound ways. Often depicted as an invisible yet ever-present force resembling a ghost, it exerts its influence quietly but significantly. It allows patients to continue their daily routines but simultaneously disrupts their future plans and aspirations. This shift in perspective prompts patients to prioritize living in the present moment with fewer expectations or long-term aspirations.[12]
A diagnosis of blood cancer profoundly affects both patients and their family members, causing disruptions within the family dynamic.[13] Individuals who have been diagnosed with the condition and their families may need to cope with difficult physical and psychological consequences, extended periods of hospitalization, multiple hospital visits, persistent distress and uncertainty, disruptions in employment, and financial difficulties.[13]
CML patients encounter difficulties in reintegrating into their professional and social lives following diagnosis and initial treatment. The most prevalent adjustment in the workplace typically involves changes in working hours, alongside modifications in job status and work pace.[14]
QUALITY OF LIFE IN CML PATIENTS
Quality of life among patients with CML may be affected in various ways: some might lose motivation and stop their treatment, others might doubt the benefits of completing their treatment, and some may become disheartened by the side effects they experience.[15] CML presents a multitude of symptoms and treatment side effects that can disrupt daily functioning and well-being. All treatments employed for the prolonged treatment of patients with CML come with inherent side effects.[9] While treatment side effects are typically mild, most patients face many years or even a lifetime of treatment. Consequently, side effects such as fatigue, skin rashes, fluid retention, bone pain, and persistent diarrhea can significantly impair the quality of life.[16]
Factors influencing the quality of life in CML patients
Patients diagnosed with CML face a diminished quality of life.[17] Several factors can influence the quality of life in CML patients [Figure 1].
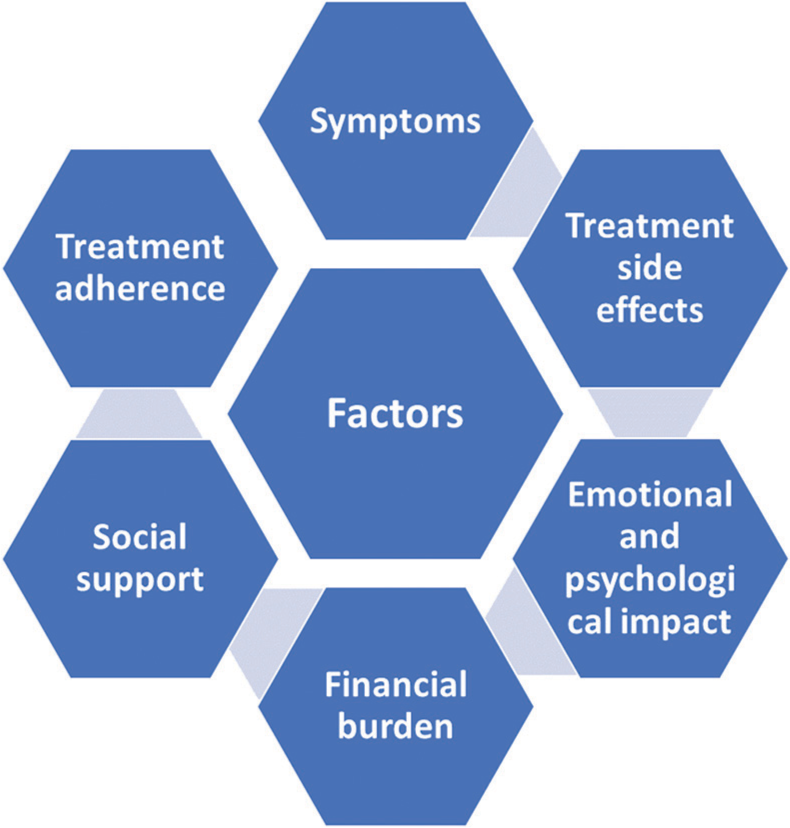
- Factors influencing quality of life in chronic myeloid leukemia patients.
Symptoms
Patients with CML might exhibit constitutional symptoms such as fatigue, weight loss, and nocturnal sweating.[7] The primary factor constraining the health-related quality of life for CML patients undergoing long-term imatinib therapy is chronic fatigue.[18]
Treatment side effects
Patients with CML undergoing treatment with TKIs often report a lower quality of life compared to healthy patients.[19] Patients treated with TKI experience side effects that not only affect the quality of life in patients with CML but also interfere with their daily activities.[20]
Emotional and psychological impact
Patients diagnosed with CML may experience emotional and psychosocial challenges, which can arise both soon after receiving the diagnosis and persist over a prolonged period.[21]
Financial burden
The expenses linked to managing CML, as well as the out-of-pocket costs connected to cancer treatment, can expose CML patients to financial strain, known as financial toxicity.[22] Patients with CML face significant financial strain in the later stages of treatment, extending beyond the expenses of targeted therapy. This financial burden is largely due to hospitalization costs, indicating a notable presence of additional health conditions among these patients.[23]
Social support
Support from family, friends, and loved ones is associated with improved psychological health in CML patients undergoing lifelong targeted therapies.[24] Enhanced social support was independently associated with lower levels of anxiety and depression, alongside elevated positive well-being, self-management, and vitality.[24] Therefore, enhancing social support networks can assist CML patients in effectively managing their condition.[25]
Treatment adherence
Increased treatment limitations and the resulting challenges could impact adherence to TKIs. Opting for a CML treatment plan that is uncomplicated and easily incorporated into patients’ daily lives could significantly influence both their quality of life and adherence.[26]
Coping strategies adopted by patients to manage physical and emotional challenges
Coping is vital for every aspect of the illness and the journey toward recovery for cancer patients, encompassing the hurdles of diagnosis, treatment, and the uncertainty surrounding prognosis.[27] Patients diagnosed with CML encountered significant treatment-related side effects, affecting their psychological and physical well-being. They developed their own strategies to handle their illness and treatment.[8] It is crucial to acknowledge and understand these coping mechanisms in interventions aimed at improving education, support, and healthcare delivery.[8] Patients outlined numerous approaches they utilized to ensure compliance with their TKI medication, including establishing routines and planning ahead, often with the aid of family support.[8]
PSYCHOSOCIAL SUPPORT FOR CML PATIENTS IN INDIA
Psychosocial behavioral interventions offer a multifaceted approach to improve the well-being of patients with chronic conditions. By effectively managing lifestyle factors and stress, providing vital social support, and imparting education on various skills, these interventions hold promise in enhancing both mental and physical health outcomes.[28] Research indicates that a higher perceived level of social support is linked to numerous positive psychological outcomes, such as decreased anxiety and depression levels, heightened positive well-being, improved self-control, and increased vitality.[24]
Moreover, patients diagnosed with chronic hematological cancers commonly express supportive care needs, particularly concerning the acquisition of information and addressing psychological concerns.[29] This highlights the importance of understanding the experiences of patients, particularly those with CML, to inform better support strategies for healthcare professionals (HCPs), caregivers, and families.[21]
The HCPs can assist patients during the initial phases of crisis and hope by offering assistance, knowledge, and comfort. As patients transition into the adaptation and establishment of a new normal, HCPs can guide them in understanding and managing the potential advantages and drawbacks of ongoing medication and disease monitoring while also encouraging them to adhere to their treatment plan.[21] Furthermore, family support is essential for managing CML at home and is positively associated with the psychological well-being of patients undergoing lifelong targeted therapies.[25]
Self-care holds paramount importance for cancer survivors, as it directly correlates with their health and quality of life. Cultural influences play a significant role in shaping both self-care practices and the factors affecting them, such as confidence levels, daily routines, motivation, social support, and the dynamics between patients and caregivers.[30] These factors influence the patient’s emotional reaction to the illness and their health-related actions concerning both prevention and treatment.[31]
Ultimately, these findings underscore the importance of a holistic approach, integrating psychosocial and familial support, in addressing the multifaceted needs of patients living with CML.
BATTLING STIGMA
Negative attitudes, stereotypes, and discriminatory behaviors toward patients diagnosed with cancer are widespread in various societies.[32] Patients may experience avoidance from others after being diagnosed with cancer, and the fear of being stigmatized can prevent them from disclosing their diagnosis.[33] This stigma is linked to increased stress associated with the illness, with numerous potential consequences.[32] Patients who are more attuned to the stigma associated with their cancer diagnosis may experience a more significant challenge to their sense of self compared to those who are less aware or sensitive to it.[34]
The stigma toward mental illness and certain cancers can cause patients to feel guilty and ashamed, potentially worsening the onset of depression.[35] Cancer-related stigma is associated with various negative impacts across different patient groups, including diminished self-esteem, increased anxiety and depression, decreased treatment adherence, delayed medical seeking, social isolation, housing limitations, employment obstacles, social exclusion, inadequate social support, and reduced quality of life.[32]
To cope with the stigma, cancer patients employ various strategies. Adaptive mechanisms, such as cognitive reframing, acceptance, drawing on religious beliefs, and disregarding negative remarks, serve to mitigate the impact of stigma on psychological well-being.[33] Conversely, some individuals resort to maladaptive coping methods, including withholding their diagnosis and avoiding discussions related to cancer, which may perpetuate feelings of isolation and hinder effective management of their condition.[33]
ADDRESSING PATIENT NEEDS: RECOMMENDATIONS AND SOLUTIONS
Improving overall outcomes in cancer care requires patient-centered strategies that prioritize the needs of the patients.[36] Patient-centered care is crucial in cancer treatment due to the increasing number of probabilistic decisions, which can lead to ambiguity and uncertainty for both doctors and patients. In addition, many cancer patients experience anxiety and distress when confronting their diagnosis and the available healthcare options.[37] By shifting the focus of CML care toward a patient-centered model, it can encourage patients to take a more active role in monitoring and managing their intake of TKIs. This change is expected to lead to better health outcomes and greater participation from patients in their own care journey.[38]
Unmet needs in hematological cancer survivor care can arise when patient support does not match the services provided. Identifying these needs, addressing them within appropriate timeframes, and utilizing strategies like peer support gatherings can enhance care models.[37] Several survivors suggested that non-profit organizations could offer additional guidance and peer support gatherings to enable survivors to access more advice regarding their care, connect with others who share similar experiences, combat feelings of isolation, and foster a sense of belonging. Survivors emphasized the importance of these sessions being conducted in-person, regularly, and in various locations to ensure optimal attendance for both survivors and their support networks.[37]
Advocacy is essential in cancer control planning and is vital in any resource context to impact policy and enhance the implementation of cancer control measures.[39] Individuals affected by cancer, including patients, survivors, and those who care for them, possess valuable perspectives on identifying deficiencies in healthcare systems. By enhancing their capabilities, their experiences serve as influential resources for promoting enhancements in knowledge, practice, policy, and services.[39]
CONCLUSION
Patients with CML in India confront significant obstacles in accessing health care and managing the burdens of the disease. Treatment side effects, stigma, and limited social support affect their quality of life. Patient-centered care, psychosocial support enhancement, and advocacy efforts are crucial to address these challenges. By prioritizing patient needs and fostering supportive networks, healthcare systems can improve outcomes for CML patients, ensuring better management of their condition and enhancing their overall well-being.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (ai)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Adherence and coping strategies in outpatients with chronic myeloid leukemia receiving oral tyrosine kinase inhibitors. Oncol Nurs Forum. 2017;44:E232-40.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence and prevalence of chronic myeloid leukemia in india over the next ten years (2017-2027) J Cancer Res Ther. 2017;13:pS292.
- [Google Scholar]
- Estimations of the increasing prevalence and plateau prevalence of chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Cancer. 2012;118:3123-7.
- [CrossRef] [PubMed] [Google Scholar]
- Recovering from chronic myeloid leukemia: The patients' perspective seen through the lens of narrative medicine. Qual Life Res. 2017;26:2739-54.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic myeloid leukemia: Modern therapies, current challenges and future directions. Blood Rev. 2021;49:100825.
- [CrossRef] [PubMed] [Google Scholar]
- Experiences of living with chronic myeloid leukaemia and adhering to tyrosine kinase inhibitors: A thematic synthesis of qualitative studies. Eur J Oncol Nurs. 2020;45:101730.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and long-term therapy in patients with chronic myeloid leukemia. Curr Hematol Malig Rep. 2016;11:80-5.
- [CrossRef] [PubMed] [Google Scholar]
- Addressing challenges faced by CML patients and physicians in SAARC countries. South Asian J Cancer. 2024;13:83-4.
- [CrossRef] [PubMed] [Google Scholar]
- A comprehensive review of chronic myeloid leukemia: An Indian perspective. J Assoc Genet Technol. 2019;45:169-74.
- [Google Scholar]
- Chronic myeloid leukemia patient's voice about the experience of treatment-free remission failure: Results from the Italian sub-study of ENESTPath exploring the emotional experience of patients during different phases of a clinical trial. Front Psychol. 2019;10:329.
- [CrossRef] [PubMed] [Google Scholar]
- "A caregiver's marriage": The impact of blood cancer on the spousal connection. Cancer Care Res Online. 2024;4:e055.
- [CrossRef] [Google Scholar]
- The impact of chronic myeloid leukemia on employment: The French prospective study. Ann Hematol. 2019;98:615-23.
- [CrossRef] [PubMed] [Google Scholar]
- Non-adherence to CML therapy and its clinical implications in India. Natl Med J India. 2017;30:142-7.
- [Google Scholar]
- Response and resistance to BCR-ABL1-targeted therapies. Cancer Cell. 2020;37:530-42.
- [CrossRef] [PubMed] [Google Scholar]
- A Survey of patient experience in CML: American and Canadian perspectives. Patient Prefer Adherence. 2023;17:331-47.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic fatigue is the most important factor limiting health-related quality of life of chronic myeloid leukemia patients treated with imatinib. Leukemia. 2013;27:1511-9.
- [CrossRef] [PubMed] [Google Scholar]
- Side effects of treatment with tyrosine kinase inhibitors in patients with chronic myeloid leukaemia and the occurrence of depressive symptoms. Contemp Oncol (Pozn). 2023;27:277-83.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective analysis of symptom burden for patients with chronic myeloid leukemia in chronic phase treated with frontline second-and third-generation tyrosine kinase inhibitors. Cancer Med. 2018;7:5457-69.
- [CrossRef] [PubMed] [Google Scholar]
- The patient journey in chronic myeloid leukemia patients on tyrosine kinase inhibitor therapies: Qualitative insights using a global ethnographic approach. Patient. 2013;6:81-92.
- [CrossRef] [PubMed] [Google Scholar]
- Financial toxicity and quality of life among people with chronic myeloid leukemia on tyrosine kinase inhibitors. J Clin Oncol. 2023;41:e18918.
- [CrossRef] [Google Scholar]
- The economic burden of chronic myeloid leukemia in patients with later lines: Findings from a real-world analysis in Italy. Adv Ther. 2023;40:961-74.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological well-being and social support in chronic myeloid leukemia patients receiving lifelong targeted therapies. Support Care Cancer. 2016;24:4887-94.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of knowledge, attitudes, and practices of CML patients and their families toward TKI therapy in China. Medicine (Baltimore). 2023;102:e36498.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic myeloid leukemia (CML): Association of treatment satisfaction, negative medication experience and treatment restrictions with health outcomes, from the patient's perspective. Health Qual Life Outcomes. 2013;11:167.
- [CrossRef] [PubMed] [Google Scholar]
- Coping in patients with hematologic malignancies undergoing hematopoietic cell transplantation. Blood Adv. 2024;8:1369-78.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived social support among patients and the contribution in the management of the chronic disease: A brief review. Series Clin Med Case Rep Rev. 2023;1:1-9.
- [CrossRef] [Google Scholar]
- Experiences and preferences for psychosocial support: A qualitative study exploring the views of patients with chronic haematological cancers. BMJ Open. 2023;13:e070467.
- [CrossRef] [PubMed] [Google Scholar]
- Cultural factors affecting the self-care of cancer survivors: An integrative review. Eur J Oncol Nurs. 2022;59:102165.
- [CrossRef] [PubMed] [Google Scholar]
- Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol. 2004;5:119-24.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer-related stigma and depression in cancer patients in a middle-income country. Asia Pac J Oncol Nurs. 2019;7:95-102.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of stigma and stigma-focused interventions on screening and treatment outcomes in cancer patients. Ecancermedicalscience. 2021;15:1308.
- [CrossRef] [PubMed] [Google Scholar]
- Identity threat and stigma in cancer patients. Health Psychol Open. 2014;1:2055102914552281.
- [CrossRef] [PubMed] [Google Scholar]
- Depression and anxiety among people living with and beyond cancer: A growing clinical and research priority. BMC Cancer. 2019;19:943.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of patient-centered care on cancer patients' QOC, self-efficacy, and trust towards doctors: Analysis of a national survey. J Patient Exp. 2023;10:23743735231151533.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the supportive care framework to explore haematological cancer survivors' unmet needs: A qualitative study. BMC Health Serv Res. 2020;20:1062.
- [CrossRef] [PubMed] [Google Scholar]
- The development of a web-based, patient-centered intervention for patients with chronic myeloid leukemia (CMyLife): Design thinking development approach. J Med Internet Res. 2020;22:e15895.
- [CrossRef] [PubMed] [Google Scholar]
- International framework for cancer patient advocacy: Empowering organizations and patients to create a national call to action on cancer. J Glob Oncol. 2015;1:83-91.
- [CrossRef] [PubMed] [Google Scholar]






