Translate this page into:
Oral cancers – Micronuclei as biomarker of genotoxicity a population-based study to establish usable dynamic cut off limits in tobacco users

*Suresh Amin, Genomic Research Centre, M S University of Baroda, Gujarat, India. suamin_2001@yahoo.com
-
Received: ,
Accepted: ,
Abstract
Buccal mucosal samples are studied for micronuclei in tobacco users. This was with emphasis in tobacco chewers. Earlier we established protocol for collecting,staining, and analyzing micronuclei (MN) in buccal smears. Samples from over 650 patients were studied for micronuclei. MN( micronuclei ) are used as a biomarker for genotoxicity in tobacco users. This was clearly evidenced by steady increase in frequency of MN from cases with no tobacco habit, cases with tobacco habit, to potentially malignant lesions (PMD )to frank malignancy in various stages. Since all tobacco ab-users do not get cancer and may take considerable time there is a need to identifying susceptible groups. Here one can arbitrarily use outliers. In the current study nearly 20 % are outliers This is a cheaper way and such cases an be subjected to further studies for some well known gene markers or these identified patient outliers can directly warned of thier greater susceptibility.
Keywords
Feulgen stain
Field application
Genotoxicity
Micronuclei
Papanicolaou
Tobacco use
INTRODUCTION
In India, 90% of all mouth cancers are oral squamous cell carcinoma (OSCC).[1-3] OSCC is most common in males in India. 5 years survival rate (56%) is poor as the patients often come in an advanced stage. Cancer is mutation induced in DNA. There are many mutations inducing substances such as viruses (HPV), lifestyle, nutrition deficiency, and chemicals (commonly known as carcinogens). Some substances like folic acid prevent mutations to an extent.
Tobacco
Among various carcinogen containing substances, tobacco is one of them. Tobacco has many chemicals. Tobacco is consumed either as smoking or smokeless tobacco (SLT). In India, SLT habit is alarmingly increasing. According to one estimate, 25% of Indians are addicted to one or other form of SLT. One sees in as young as 10 years of age and rural as well as urban areas. Tobacco is both genotoxic and cytotoxic.
Micronuclei (MN) Biomarker
To study and warn tobacco users one needs to have biomarkers. Assessment of biomarkers should be cheap, widely available, reliable, without much infrastructure, and easily trainable man power.
Presence of MN in the cell cytoplasm and an increasing number of cells with MN are studied extensively by many groups. In 1998 and 2008 in an international collaborative study (human micronuclei [HUMN]),[4,5] over 30 laboratories in over 30 countries participated, and one of the conclusions was that MN in buccal smears is a useful marker to study the genotoxic effect of tobacco abuse.
Tobacco abuse induces in many cases pre-cancer or potentially malignant disease (PMD). These oral submucous fibrosis, leukoplakia, and erythroplakia are clinical conditions.
The assessment of MN in exfoliated cells to study genotoxicity, cytotoxicity is a promising tool for the study of epithelial carcinogens.[2,4]
There are several papers that show the utility of buccal MN in screening in oral cancers and pre-cancers.[2-11] There is an international collaborative study on HUMN.[4,5] In HUMN study, over 30 laboratories participated as collaborative laboratory. Every year there is an increasing number of papers and labs adopting MN studies.[5]
SLT and Need for Biomarker
At present, there is alarmingly widespread usage of many varieties of SLT such as - Gutka, Kaini, Mava, and Snus. The habit is seen in India as well as in neighboring Southeast Asia countries such as Bangladesh, Sri Lanka, Indonesia, and Thailand. The SLT habit is both rural and urban and increasingly seen in younger age groups, school-going children. One sees the habit in poor working class women too.
Importance of MN has been well recognized in the study of cytotoxicity and genotoxicity.[2,3,6-8]
Since the use of tobacco is known to be genotoxic[4] and cytotoxic, we need to objectively forewarn tobacco users. This is easier said than done. In spite of massive campaigns, the use has not abetted but is seen to be increasing, particularly in the rise of SLT users.
To study these adverse effects of toxic chemicals, one needs to have a surrogate marker of biomarkers. A biomarker has been defined as a characteristic that is objectively measured and evaluated as an indicator of a normal biological process, pathogenic processes or pharmacological responses to therapeutic intervention or other health-care interventions.[5] MN as a biomarker in cancer research has been part of the international collaborative study.[4,5]
MATERIALS AND METHODS
Selection of Patients
Ethics committee permission was taken from Medical College Baroda and Medical College Karamsad. Patients coming to OPD clinic of teaching hospitals were asked about tobacco habit (SLT) and were randomly selected, and permission to take buccal smear was asked. Most patients come from in and around Vadodara and Anand, Gujarat. They came from rural, poor, and educationally poor background. We have consciously tried not to include smokers. There is a standard form for information on patients, and this is to be filled and submitted with samples. Collection protocol, staining, and examination were done as per the previous paper.[1]
Ten codes were arbitrarily adopted. Code 0 meant no clinical lesion and no h/o tobacco usage. Code 1–3 represented no clinical lesions but the duration of habit 5 years, 5–10 years, and more than 10 years. Code 4–6 represented clinical disease. Code 4 - SMF of various grades, Code 5 - is leukoplakia, Code 6 - associated erythroplakia. Code 7–9 was for clinically malignant. Code 7 - was for clinically suspicious malignancy, Code 8 - was for clinically malignant, Code - 9 was for clinically malignant with metastatic nodes. Code 10 was melanoplakia and other lesions.
Acquisition of Picture and Data Analysis
Trinocular light microscope with Magcam camera and MagVision software with picture acquisition facility was used for the study. First, one uses ×10 objectives to locate the appropriate field of interest and then used ×40 for the picture acquisition and with standard zigzag fashion and so as not repeats the same field. Images, thus, acquired are saved in the respective folders for further analysis and MN counting, recounting.
RESULTS
There is the evident rise of MN [Figure 1 and Table 1] - from no habit and no lesion to PMD lesions and frank malignancy in different stages.
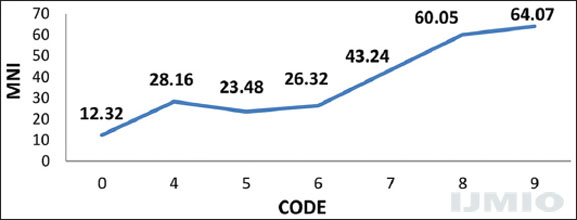
- Micronuclei index, in people with no tobacco habit - (code 0), tobacco habit with potentially malignant lesions (code 4–6) and frank cancer in various stages (code 7–9)
| SR No | Code | Total | Mean MN/1000 | 1 SD/2 SD | Range | Number of cases above >2 SD |
|---|---|---|---|---|---|---|
| 1 | 0 | 73 | 12.32 | 10.83/21.66 | 1.49–23.15 | 8 |
| 2 | 1 | 56 | 17.91 | 12.57/25.14 | 5.34–30.48 | 10 |
| 3 | 2 | 10 | 14.0 | 7.7/15.4 | 6.3–21.7 | 4 |
| 4 | 3 | 25 | 27.67 | 17.22/34.44 | 10.44–44.88 | 5 |
| 5 | 4 | 97 | 28.57 | 15.66/31.32 | 12.87–44.19 | 30 |
| 6 | 5 | 103 | 23.42 | 17.12/34.24 | 6.3–40.54 | 14 |
| 7 | 6 | 39 | 27 | 25.26/50.52 | 1.7–52.26 | 4 |
| 8 | 7 | 58 | 47.63 | 24.98/49.96 | 22.65–72.61 | 24 |
| 9 | 8 | 22 | 48.13 | 31.63/63.22 | 16.52–79.74 | 7 |
| 10 | 9 | 23 | 51.14 | 45.49/90.98 | 15.91–106.89 | 5 |
| 11 | 10 | 132 | 21.45 | 14.21/28.42 | 7.2–35.66 | 27 |
| Total | 638 | 146 |
MNI: Micronuclei index
The data show that the frequency of MN increases with age, and then declines by the 6th decade as shown in Figure 2.
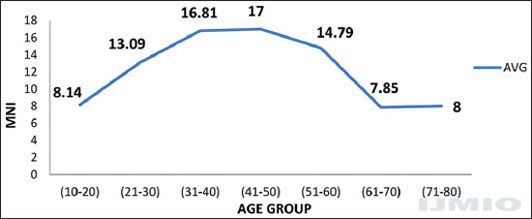
- Mean micronuclei index for various age groups (no tobacco habit)
It appears that tobacco damage as evidenced by MN plateaus of after 10 years as seen in Figure 3.
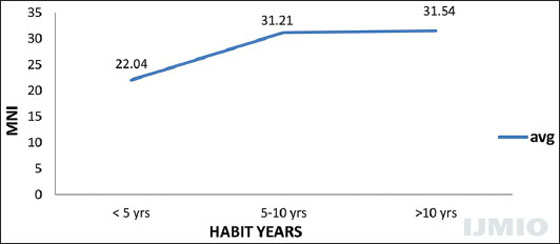
- Tobacco habit duration and micronuclei
Data in Figure 4 shows that the habit of smokeless tobacco, as well as smoking, potentiates nuclear damage, with a synergistic effect in those with both habits.
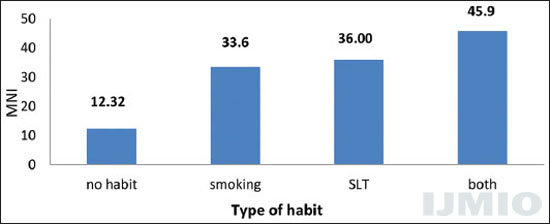
- Micronuclei index in individuals with no habit, smoking alone, smokeless tobacco alone or both
DISCUSSION
How are MN Formed?
MN are small extranuclear DNA particles formed when chromosome fragments in dividing cells do not get incorporated in the nucleus of a daughter cell.[5] This may arise from unrepaired dsDNA break, suggesting that repair pathways may have become errant. Malsegregation of the whole chromosome can occur during anaphase, and this can be due to hypomethylation of cysteine in centromeric and pre-centromeric repeat sequences. In oral mucosa, the squamous epithelium is 6–7 layers. Damage due to tobacco occurs in a basal layer which has dividing cells. MN forms due to lack of integration in a single nucleus occur here, and subsequently, these cells migrate upward. During migration, some cells die and fail to reach up. One counts MN in these superficial shedded cells. There are several techniques to stain MN.[11,12] These are either DNA specific (Feulgen, fluorescent acridine orange, 4,6- diamini2-phenylindole, propidium iodide, and FISH - centromere, tubulin) or nonspecific such as Geimsa, H and E, May Grunewald, and Papanicolaue (PAP). There are comparative studies between the two types of stain. Results may vary, but it cannot be overemphasized that collection and procedures in processing matter highly.[1] There are many chromatin bodies in various stages in the cytoplasm. The combined criteria of Heddle and Countryman (1976) and Tolbert’s et al.[7] are what we have considered to characterize MN.
Tobacco abuse is widespread in India and South East Asia. For any technique that one wants to propagate on a wider scale, it has to be low capital intensive, reproducible at the hands of average skilled technicians, technologically reliable, affordable, and useful. MN has been used to study the cytotoxic and genotoxic effect of various substances; this is as a research tool at present. We recommend that optimal use of MNI would not be for diagnostic of early cancer, but rather for screening purposes.
As is known all tobacco chewers and smokers do not get cancer. All oral cancer cases cannot be attributed to tobacco. Some OSCC does not have a history of tobacco usage. Equally true is large number of people with OSCC cases having a history of tobacco. Is it possible to use molecular markers in selected cases. One option is to use MN index (MNI), to narrow down selection.
Like all screening, the results are pointers and have to be used judiciously. So far buccal MN screening, as epidemiology, sociology, and clinical diagnostic laboratory tool have not been widely adopted. Papanicolaou (popularly known as PAP stain) has been widely accepted and used for cervical cancer screening. This can be adopted for oral cytology screening as we have shown previously. This is particularly so in oral lesions related to tobacco (smoking, chewing, and even in snuff users). The studies, however, vary in many details, consistency, and rarely taking a sample size of over 100. One needs to establish a range for various groups and geographic area. In most studies, this is insufficient for using as comparative guidelines in clinical practice.
Table 1 and Figure 1 show clear evidence of rising MNI from no tobacco users to PMD (pre-cancer) to cancer in various stages. If one uses 2 SD values for MNI then we can narrow down our focus on these people - for motivation to quitting as well as subject them to panel of established molecular markers.[13-16] MNI could also be objectively used by social workers in persuading tobacco abusers to leave tobacco habit. Like PAP stain in cervical smears, one can use PAP stain in oral cytology for determining MNI. This will be affordable and can be used in mass camps.
Acknowledgment
We thank Dr. Pinakeen Patel of Bill biotech and RBL for encouraging. We thank Prof Dr. Ranjan Aiyer ENT Department of SSG Hospital and Baroda Medical college, Dr. Girish Mishra Prof and head of ENT Department of Medical college in Karamsad for assigning two of their PG residents, Dr. Aniruddha Wagh and Dr. Tanay Parikh for ethical liaison. The study was initiated and carried out by late Dr. Bharat Chattoo in his Genomic Research Centre, MS University of Baroda. Thanks are to Dr. Radhika Vaishnav for persistent valuable help and insights in preparing this manuscript.
REFERENCES
- Suitability of papanicolaou stain for micronuclei mass screening in buccal smears comparing reference feulgen stain and papanicolaou stain in field. Int J Mol Immunooncol. 2018;3:73-7.
- [Google Scholar]
- Burden of cancer and projections for 2016, Indian scenario: Gaps in the availability of radiotherapy treatment facilities. Asian Pac J Cancer Prev. 2008;9:671-7.
- [Google Scholar]
- GATS-2 Global Adult Tobacco Survey Fact Sheet India :2016-17.
- Clinico-pathological correlation of micronuclei in oral squamous cell carcinoma by exfoliative cytology. J Oral Maxillofac Pathol. 2008;12:2-7.
- [CrossRef] [Google Scholar]
- The micronucleus assay in exfoliated cells of the human buccal mucosa. Mutagenesis. 1987;2:11-7.
- [CrossRef] [PubMed] [Google Scholar]
- Micronuclei and other nuclear anomalies in buccal smears: A field test in snuff users. Am J Epidemiol. 1991;134:840-50.
- [CrossRef] [PubMed] [Google Scholar]
- The human micronucleus project–an international collaborative study on the use of the micronucleus technique for measuring DNA damage in humans. Mutat Res. 1999;428:271-83.
- [Google Scholar]
- The micronucleus assay in human buccal cells as a tool for biomonitoring DNA damage: The HUMN project perspective on current status and knowledge gaps. Mutat Res. 2008;659:93-108.
- [Google Scholar]
- Quantitating the synergistic effect of smoking and alcohol consumption with the micronucleus test on human buccal mucosa cells. Int J Cancer. 1983;31:305-8.
- [Google Scholar]
- Feulgen staining remains the gold standard for precise DNA image cytometry. Anticancer Res. 2011;31:53-8.
- [Google Scholar]
- Comparison of the papanicolaou and feulgen staining methods for DNA quantification by image analysis. Cytometry. 1990;11:468-74.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of staining procedures on the results of micronucleus assays with exfoliated oral mucosa cells. Cancer Epidemiol Biomarkers Prev. 2006;15:1835-40.
- [Google Scholar]
- Identification of upregulated genes in oral squamous cell carcinomas. Head and Neck. 2012;35:10.
- [Google Scholar]
- Prognostic and predictive markers for oral squamous cell carcinoma: The importance of clinical, pathological and molecular markers. Saudi J Med Med Sci. 2014;2:12.
- [CrossRef] [Google Scholar]
- Analysis of angiogenic markers in oral squamous cell carcinoma-gene and protein expression. Head Face Med. 2015;11:19.
- [CrossRef] [PubMed] [Google Scholar]
- Cell proliferation markers in oral squamous cell carcinoma. J Mol Biomark Diagn 2012:S2-6.
- [Google Scholar]






